2. Our First Guide
A PREVIEW CHAPTER of The Wilds of Cancer
Unknowingly, I began my journey into the wilds of cancer well before I received my diagnosis. Two months earlier, Mary and I were on a guided rafting and hiking trip through the Grand Canyon. The guide was essential. We weren’t skilled in handling the ever-changing water conditions and didn’t know the trails we hiked on. The guide gave us direction and reassurance.
While the guided days were fun, the nights in the canyon were troubling. I awoke so many times to urinate that I wondered what was wrong. The nighttime busyness continued in a motel after the trip ended. Concerned, I recorded my liquid input and output for several days and took the record to a scheduled annual exam with my primary care doctor once we returned home to Montana. I discussed the data and my worries with her. She ordered urine and blood labs. The urine lab showed no irregularities. However, the blood work revealed the PSA score that started this journey.
PSA stands for prostate-specific antigen, a protein produced by normal—and malignant—prostate gland cells. A PSA score is measured in nanograms per milliliter but is usually abbreviated to just the number. Most doctors look for a PSA of four or higher when deciding whether to test for prostate cancer. My score was twenty-five.
That high score shocked me into researching PSA testing. I was surprised to learn that my doctor could have justified not testing. I found a section of the American Urological Association website that presented a prostate cancer curriculum for medical students and described varying accepted standards. One stated that men over seventy and in excellent health may benefit from testing. Another recommended no testing for any men seventy and older. Since I was seventy-three, I was thankful to have a doctor who requested a PSA test, studied the results, and referred me to my first urology consult.
Mary immediately volunteered to accompany me. I treasured her willingness to attend, listen, and question since we could have different takeaways from deep discussions.
When we walked into that initial urology consult, I hoped to find a guide for this journey into unknown territory. I was determined to ask the urologist where he stood on treating prostate cancer in “a man my age.” In the last few years, I’ve grown to dislike that expression, but it fits. Before we began, I asked the urologist, “Can I record our conversation?”
“That’s a good idea,” he said. He went on to explain that prostate cancer can be found in up to seventy-five percent of men my age and older. My lack of symptoms was expected. He would typically not see symptoms until the cancer was far advanced. With my PSA of twenty-five, he gave me a fifty-fifty chance of having prostate cancer.
He asked if I had had PSA tests during previous annual exams. He wanted to look for a baseline or changes in the PSA number over time. A rise could increase the odds that I had active cancer cells in my prostate and that further testing was needed. As I explained that I had been healthy my entire adult life and rarely visited a doctor, I finally admitted to myself that missing numerous annual exams and PSA tests was a mistake. I knew that Mary agreed I had made a mistake since she had repeatedly encouraged me over the years to have PSA tests.
I told the urologist I had read that treatment for prostate cancer was not always recommended for men over seventy. He said the current thinking was that men my age had so few years left to live on average that something else would likely take us before prostate cancer. Testing and treatment, which are expensive and could have troublesome side effects, might not be called for.
He gestured toward me with his tattooed arm. “But look at you, you’re physically fit, not overweight, and on no medications. You have a good ten to twenty years left. Why not treat you?”
I smiled and silently calculated that perhaps I could have more years with Mary, our kids, and our granddaughter. A statistic I uncovered boosted this hope: while prostate cancer was common, of those diagnosed, only about one man in six died from the disease. Five of six didn’t. I could live, no pun intended, with those odds.
The urologist said that an accurate diagnosis required a biopsy. He would take samples from my prostate and send them to a lab that would determine if cancer cells were present and how aggressive they were. He would call me with the results. I agreed to schedule a biopsy appointment.
As the initial consult ended, I realized we had found our first guide. This guide would be as essential as the one who led us through the Grand Canyon. Mary and I needed guidance in handling the ever-changing medical information. We did not know the medical trail we would travel or how long we would be on it. We would look to this guide, and perhaps others, for direction and reassurance.
Order your PREPUBLICATION COPY of The Wilds of Cancer: A Life-Affirming Journey.
To read another PREVIEW CHAPTER.
P.S. If you found this post helpful, would you please consider restacking it and sharing it with your audience?
Click the button to subscribe to this Substack for free. I hope you join me, and I welcome your comments and feedback.
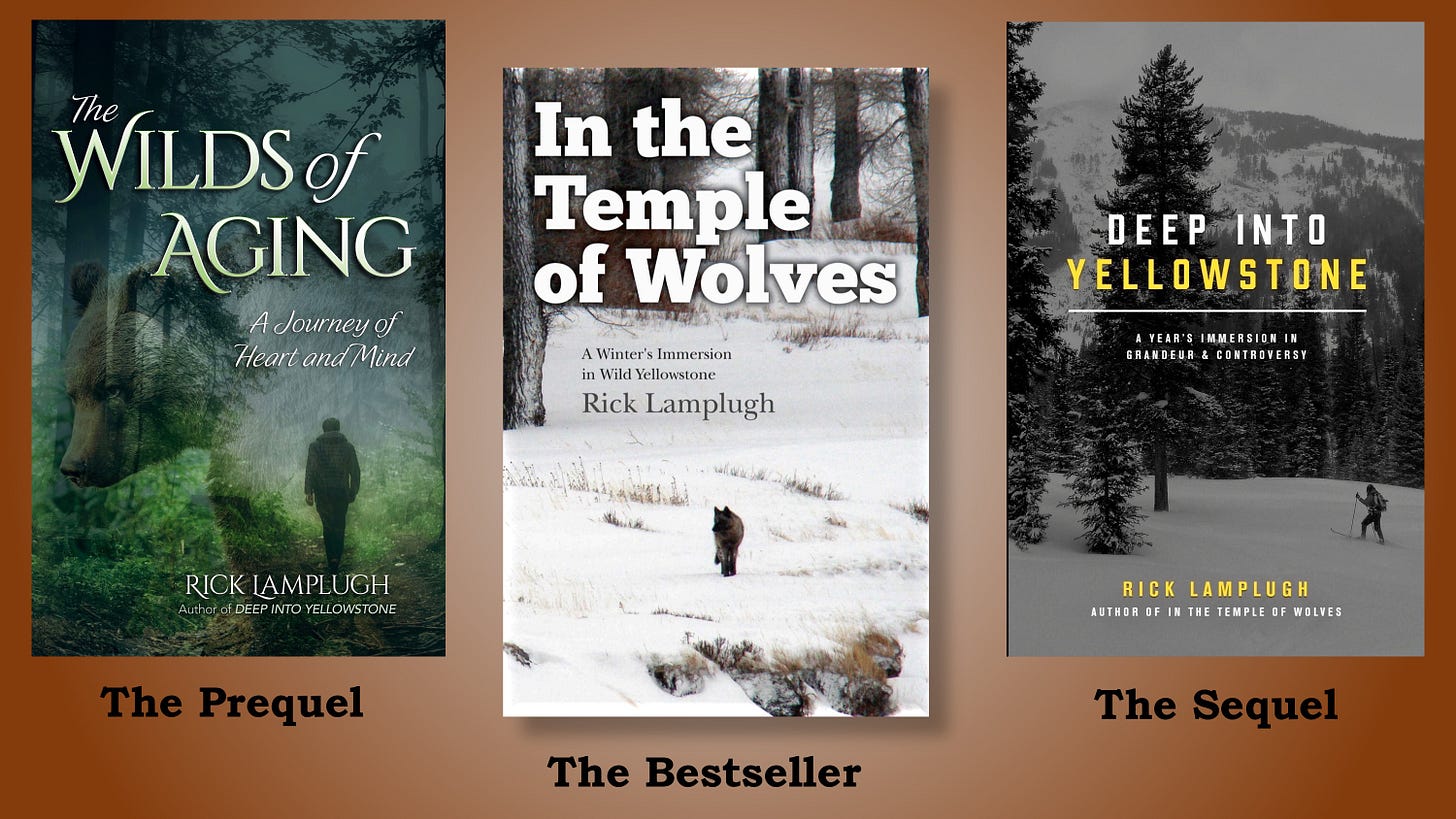
For stories of moments Mary and I have shared in wild lands and with wildlife, check out my previous books. In the Temple of Wolves is the bestseller with more than 500 five-star reviews on Amazon. Deep into Yellowstone is the sequel and won a Gold Medal in the Independent Publisher Book Awards. The Wilds of Aging, the prequel and winner of a National Indie Excellence Award, takes you on a journey with me into wild lands and aging. Click on a title for a signed copy, or visit Amazon for unsigned paperback copies, ebooks, and audio CDs.
Disclaimer
I’m a writer, not a doctor. I’m very qualified to write stories about my journey. I’m not qualified to give—nor am I giving—medical advice. As these stories show, Mary and I came up with many approaches to deal with my cancer. We always ran our ideas by our medical team to see how the approaches fit medically. Everybody’s body is different. What worked for me may not work for someone else. If something in these stories generates an idea of an approach that you or someone you know might use, first consult with the medical team.



Hi Rick and the wife Mary ,
I too am currently being treated for Prostate cancer .
I got very worried about you and was wondering what had happened to you - Glad your ok . I am doing ok also , My PSA level is as low as it can get at 0.01> but i am taking hormone treatments for about another year yet . I'll talk some more later - just so glad to hear from you again . God Bless you both .
Thank you so much for sharing your journey. Your feelings about "a man my age" resonated, although for me, it is "a woman your age should" blah, blah, blah.... I truly dislike the assumptions. :)
I look forward to reading your next chapter.